You are an accountant, and you have no experience in medicine. You visit your primary care office for a routine checkup on a Wednesday afternoon to see how your blood pressure is coming along after starting a new medication.
“You will be seeing the PA today; is that okay?” the medical assistant asks. You respond in the affirmative, quite frankly not knowing the difference between the numerous medical providers in the office. “I think I saw a Nurse Practitioner last visit” you think to yourself. But really, you are not sure what any of it means. Doctors, nurses, nurse practitioners, physician assistants, medical assistants… what’s the difference?
For our patients, the experience detailed above can be very common and quite confusing. Oftentimes, the most confused roles are those of nurse practitioners and physician assistants. Nurse practitioners sometimes get confused with registered nurses, while physician assistants often get mistaken for medical assistants.
We can say “Oh, they are both advanced practice providers,” but this can muddy the waters even more. Physician assistants and nurse practitioners are similar in many ways, and different in others. So how can we explain the difference between the two to our patients and describe exactly what we do?
It is sometimes helpful to describe where the differences arise between these two professions to really appreciate how similar they are.
Back to School
One of the main differences between nurse practitioners and physician assistants lies in their differing educational programs.
Physician assistants are trained in medicine based on the medical model. This is the same model that is used as a framework for physician education.
This method of instruction traditionally takes a more mechanistic view of the body and the diseases that can occur within it. It looks at different diseases, their interruptions to various organ systems, and the treatment and/or prevention of these diseases. While this description is simplistic, it provides a good idea of the general style of medical education for physician assistants.
Physician assistant training programs almost universally award a Master’s degree. The programs are typically 24-25 months long and are full-time. Most programs require 2000 or more patient care experience hours to be accepted for admission. This experience can be from many different areas, but often is acquired by prospective students working as medical assistants, radiology technicians, patient care technicians, EMTs, or even nurses.
Nurse practitioners are trained in programs based on the nursing model. This model emphasizes a holistic approach to patient care and treatment. Paramount of importance in this training method is the whole patient. This includes chronic conditions, socioeconomic status, social supports, individual needs, and patient independence.
Nurse practitioners usually are required to work as registered nurses before being accepted into a nurse practitioner program. While there is no uniform number of years required to be accepted into all programs, most schools recommend at least a few years of practice as a nurse.
There are a few different degree paths for nurse practitioners, based on the specialty in which they wish to work. These include both Masters and Doctorate level programs.
While the medical model and nursing model have their differences, it is important to note that physician assistants and nurse practitioners both receive holistic, comprehensive, patient-centered, and evidence-based training. The education is more similar than it is different.
The Chef’s Specialty
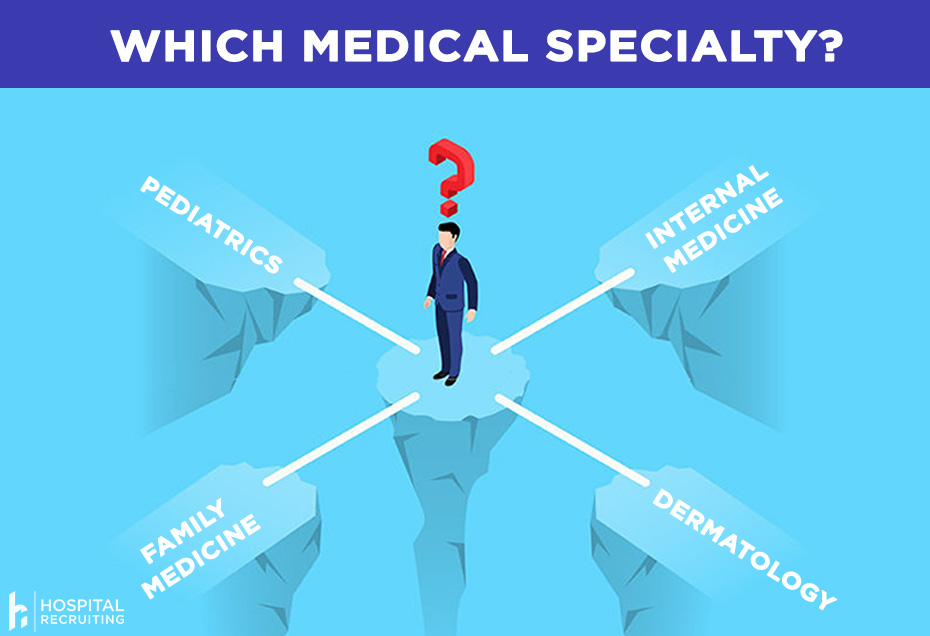
Another important distinction between physician assistants and nurse practitioners is in their respective areas of specialty and the degree needed to practice in that specialty.
For physician assistants, the question of specialty is often an easy one to answer. Because the education for physician assistants is generalized and based on the medical model, they are legally licensed to practice in almost all medical specialties.
With this is mind, PAs are seen more often in surgical or acute care specialties, due to a higher educational emphasis on procedures when compared to nurse practitioner programs. This is only a generalization, however, as many PAs practice in specialties like primary care, cardiology, or nephrology.
With this in mind, it is important to understand that nurse practitioners actually have different degree paths for different specialties.
First, there is the Family Nurse Practitioner (FNP). This type of NP specializes in treating patients from birth through adulthood. FNPs typically work in primary care and help to manage acute and chronic medical conditions.
Second, is also the Pediatric Nurse Practitioner (PNP) that is licensed to specifically work with and treat children from birth to age 22. PNPs typically work in pediatric primary care offices.
There is also the Psychiatric Nurse Practitioner. This type of NP works in both outpatient and inpatient psychiatric settings to manage acute and chronic psychiatric conditions.
While a large portion of nurse practitioners in the workforce today are FNPs, PNPs, and Psychiatric NPs, there is a host of other types of nurse practitioners. These include Oncology Nurse Practitioners (ONP), Occupational Health Nurse Practitioners (OHNP), Acute Care Nurse Practitioners (ACNP), Neonatal Nurse Practitioners (NNP), Women’s Health Nurse Practitioners (WHNP), and Geriatric Nurse Practitioners (GNP).
I Feel Like There is Someone behind Me?

One important difference between PAs and NPs is in oversight requirements.
While physician assistants currently are required by law to have physician oversight in all 50 states and Washington D.C., nurse practitioners only require this type of oversight in 27 states. In all the other states, they can legally practice independently.
For PAs, this supervision takes the form of a delegation agreement, also called a practice agreement. This legal form outlines exactly what PAs can do in their own practice, how they can practice, supervision requirements by their supervising physician, and prescription authority. This document is legally binding and required for a PA to be able to practice in all 50 states and Washington D.C.
Even though PAs need physician oversight, this does not mean that a physician must be always supervising them. A physician does not even need to be on site, so long as they are available for consultation if needed. Though individual practice varies, physicians must be onsite for a specified number of days every year and provide guidance/supervision on demand as required by the PA.
Nurse practitioners in one of the states requiring oversight must have a collaborative agreement in place with a supervising physician. This document is very similar to the delegation agreements used by physician assistants, with many of the same legal requirements and regulations.
In one of the states not requiring oversight, nurse practitioners are fully licensed to practice independently without physician supervision or collaborative practice agreements in place. NPs in these states even have the ability to open their own practices.
More Similar Than Different
While this post mainly details the differences between PAs and NPs, there really are more similarities than differences between these two wonderful professions. Both PAs and NPs provide exceptional patient care to patients of all ages in almost all settings.
There is a reason that patients sometimes confuse physician assistants and nurse practitioners: because they are both great! Both professions receive exceptional training from incredibly diverse backgrounds, and they provide patient care in a cost-effective and evidence-based manner.
**Editor’s Note: If you liked this article, be sure to check out our other advanced practitioner resources**
